Abstract
Introduction POEMS syndrome (polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy, and skin changes) is a rare plasma cell dyscrasia. The treatment of POEMS syndrome has not been standardized and systematic therapies include autologous stem cell transplantation (ASCT), melphalan, immunomodulatory drugs (IMiDs) and protease inhibitor (PI)-based chemotherapy. Lenalidomide with dexamethasone (Rd) can lead to rapid hematological and neurological responses, however, progression-free survival (PFS) after Rd treatment remains unsatisfactory. This study aims to assess the effect of lenalidomide maintenance on the progression-free survival of POEMS patients after first-line Rd therapy.
Methods Patients who were newly diagnosed with POEMS syndrome between 1 January 2012 and 31 December 2020 and had completed 12 cycles of Rd as a first-line therapy were included. Data were extracted from a prospectively maintained database. After first-line therapy, the patients in the maintenance group received single-agent lenalidomide daily on d1-21/28 d for another 12 months or until disease progression/relapse or intolerance. PFS was defined as the time from maintenance/observation to VEGF relapse, the deterioration of clinical symptoms, or death. Subgroup analysis was performed to explore the preferred subgroup for maintenance therapy.
Results A total of 128 patients receiving lenalidomide as maintenance therapy (n=59) and under observation (n=69) were included. A total of 63.3% of the patients were male, and the median age at diagnosis was 53 years (range, 24-75). Overall, 25.3%, 45.3%, and 29.5% of the patients were at low, medium, and high risk, respectively, with no significant fundamental difference in the two groups.
During maintenance or observation, the hematological CR (CRH) rate increased from 46% at the end of Rd treatment to 54% in the maintenance group and from 50% to 53% in the observation group. The VEGF CR(CRV) rate increased from 55% to 67% in the maintenance group and from 46% to 51% in the observation group. Regarding neurological responses, durable neurological remission was observed in 16 patients (76.2%) in the maintenance group and 26 patients (72.2%) in the observation group.
With a median follow-up time of 48.9 (IQR 23.7-68.2) months from the initiation of maintenance or observation, the median progression-free survival was 47.9 months in the maintenance group and 36.4 months in the observation group (HR 0.63, 95% CI 0.38-1.07). The five-year overall survival rate was 95.5% and 93.6% (HR 0.87, 95% CI 0.17-4.6), respectively.
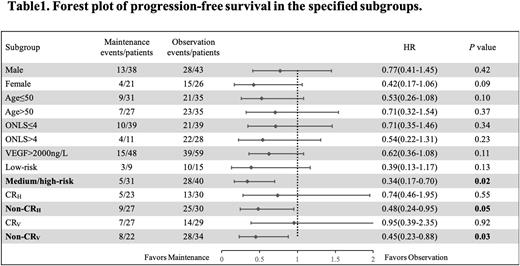
In subgroup analysis (Table 1), medium- to high-risk patients who received maintenance therapy had significantly longer progression-free survival than those who did not (median PFS: not reached vs. 35.0 months, HR 0.34, 95% CI 0.17-0.70). In addition, in patients who did not achieve CRH after Rd therapy, the median progression-free survival was 42.6 months in the maintenance group compared to 17.8 months in the observation group (HR 0.48, 95% CI 0.24-0.95). Similar results were also seen in patients who did not achieve CRV (median PFS: 25.2 vs.12.8 months, HR 0.45, 95% CI 0.23-0.88).
Conclusion Maintenance therapy with lenalidomide is a practical approach to increase responses and reduce the risk of progression, especially in high-risk patients and in those with inadequate remission. Maintenance therapy may be considered part of the standard therapy in these patients in POEMS syndrome.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal